Background: Pregnancy is a known hypercoagulable state. Traditionally, pregnant patients with high risk thrombophilias, which include homozygous Factor V Leiden (FVL), homozygous prothrombin gene variant (PGV), antithrombin deficiency, and double heterozygotes for thrombophilia are treated prophylactically with anticoagulation due to their significantly increased risk of venous thromboembolism (VTE). However, for pregnant patients with mild-risk thrombophilia, which include heterozygous FVL and heterozygous PGV, VTE risk is lower and VTE prophylaxis is not typically recommended and decision to use anticoagulation is typically left to the physician's discretion based on each patient's individual risk factors. To date, there is not a systematic review or meta-analysis which reviews recommendations for VTE prophylaxis in the antenatal and postnatal periods in patients who are pregnant with known mild thrombophilia. The aim of this meta-analysis is to assess the association of thromboprophylaxis in prevention of obstetric complications and pregnancy-related VTE in women with known mild-risk inherited thrombophilia: heterozygous FVL or PGV, Protein C and S deficiencies.
Methods: The Medline, Embase, Lilacs, and the Cochrane Central Register of Controlled Trials (Central) was searched from inception to October 7, 2022. Identified studies were then screened by reviewers for inclusion. Inclusion criteria considered pregnant patients (antenatal) up until 6 weeks post-delivery or miscarriage (puerperium) with a known mild risk inherited thrombophilia (heterozygous FVL or PGV, Protein C or Protein S deficiency), receipt of thromboprophylaxis in either the antepartum, puerperium period, or both (prophylactic and intermediate dosing of LMWH or UFH, low-dose aspirin, or a combination of these). Control group was defined as pregnant patients with known mild thrombophilia who did not receive thromboprophylaxis in the antenatal and puerperium periods. Primary outcome was defined as VTE-related mortality and all-cause mortality, and secondary outcome was defined as adverse effects (including VTE, maternal and fetal complications, bleeding events). Statistical analysis was performed using OpenMeta[Analyst].
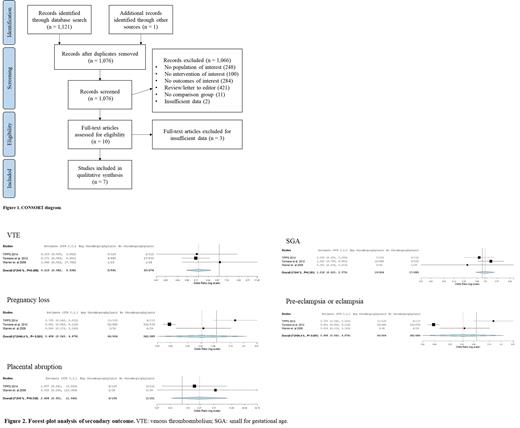
Results: In total 1,121 publications were identified through the database search, and one additional publication was identified through manual search. After screening processes by two separate reviewers, seven full text studies were determined to meet inclusion criteria and were used for data extraction and analysis. (Figure 1) Across the studies included, no events of VTE-related mortality or all-cause mortality were reported. Three studies, with a population of 1265 women, were amenable for meta-analysis of VTE and adverse events. Results showed an association with thromboprophylaxis and decreased risk of VTE (OR 0.210, 95% CI 0.082-0.538, p-value 0.001) (Figure 2). Adverse outcomes of pregnancy loss, small for gestational age (SGA), and pre-eclampsia or eclampsia were not statistically different between pregnant women who received thromboprophylaxis versus those who did not.
Discussion: Results of this meta-analysis show an association between thromboprophylaxis and decreased risk of VTE events when compared to no thromboprophylaxis in pregnant women with mild thrombophilia. Adverse outcomes did not appear to be different in those pregnant women who received thromboprophylaxis. Limitations of this study include heterogeneity of different thromboprophylaxis modalities among study designs, limited data on mortality and other adverse effects including bleeding and fetal complications. Although results of this meta-analysis were able to detect a decreased risk of VTE with exposure to thromboprophylaxis, further prospective studies are needed to establish the safety of thromboprophylaxis in that population.
Disclosures
Rojas Hernandez:Anthos Therapeutics: Research Funding.